What is the FibraValve, and why was it designed in the first place? Here’s the Why: Strep throat is a common childhood illness in the United States, but in less wealthy countries, it can lead to rheumatic fever, a condition that causes inflammation and can damage the heart valves. To address this problem, a team led by Kevin Kit Parker at the Wyss Institute and Harvard’s John A. Paulson School of Engineering and Applied Sciences has developed an implantable heart valve called FibraValve that grows with a child, reducing the need for invasive surgeries.
The Synthetic Heart Valve can be manufactured in under 10 minutes
The FibraValve represents a significant advancement in the field, as detailed in a recent research publication in Matter. The researchers utilized a new method called focused rotary jet spinning (FRJS) to manufacture the synthetic heart valve in under 10 minutes. FRJS allows for customization of the valve’s shape and properties down to the nanoscale, and the valve has shown promising results in studies involving living cells in vitro and in large animal models.
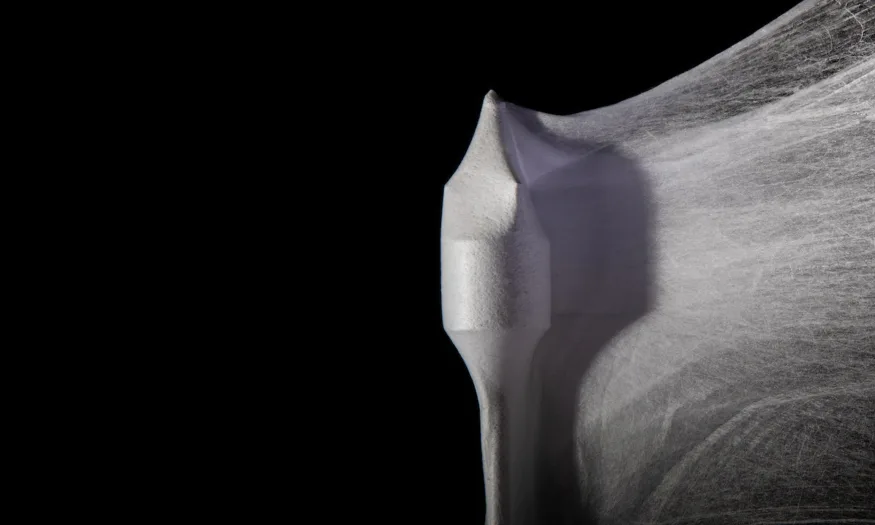
The goal of the FibraValve is to provide a blueprint for the patient’s native cells to regenerate their own living valve tissue. By using FRJS, the team hopes to not only address valve diseases in children but also establish a platform for fabricating other medical devices in the future. The innovative manufacturing process involves extruding a biocompatible synthetic polymer through a nozzle and spinning it into long nanofibers, which are collected on a heart-valve-shaped mandrel to create the valve.
The team’s previous synthetic heart valve, JetValve, demonstrated successful implantation in a sheep’s heart and the regeneration of new tissue on the device. Building on this achievement, the researchers focused on improving various aspects of the valve, including manufacturing, fiber material, and geometric design. By incorporating streams of focused air into the polymer-extruding process, they developed FRJS to enhance the rate of fiber deposition and improve the valve’s final shape.
In addition, the team used a new polymer material, called PLCL, to enhance cell infiltration once the FibraValve is implanted. The PLCL FibraValves proved to be softer and more elastic than their predecessors. The researchers optimized the geometry of the valve’s inner leaflets to minimize blood leakage, successfully reducing the leakage rate from approximately 30% to about 13% with their improved design.
To assess the performance of the FibraValve, the researchers implanted it into a living sheep’s heart using minimally invasive surgery. The valve exhibited immediate functionality, with its leaflets opening and closing synchronously with each heartbeat. Over the course of just one hour, the team observed the infiltration of red and white blood cells as well as the deposition of fibrin protein on the valve’s porous scaffolding. The implantation process caused no damage or issues.
The team plans to conduct longer-term animal testing to further evaluate the FibraValve’s regenerative capabilities and performance. They believe that FRJS has the potential to create a wide range of implantable devices, such as other valves, cardiac patches, and blood vessels.
RELATED:
- The Thinnest Computer Chip: Researchers Develop World’s First Functional 2D Microchip
- New 3D Bioprinter Can Repair Tissues From the Inside, Avoiding Major Surgeries
- Best Nintendo Switch Games in 2023
(Via)